Case Study: Aromatherapy in Long-Term Care
I journeyed into the mainstream healthcare system in 2013. At the time utilizing aromatherapy as a non-pharmacological option in senior care was rare. However, evidence was emerging to support its efficacy and I happened upon an opportunity to put my essential oils to the test.
I began working with an ambitious and compassionate director of nursing (DON) for a large long-term care center in Minnesota. She was interested in using essential oils and blends with their population. They had already attempted some aromatherapy on their own but with mixed results. A full floor was devoted to memory care residents. Several residents had advanced Alzheimer’s disease and dementia, exhibiting extreme symptoms that were not responding well to the current medication protocols.
After a discussion with the DON, we concluded we would address anxiety, mood, sleep, focus and appetite. We also addressed cravings for an alcoholic and an unique issue for a WWII survivor. We replaced their collection of “aromatherapy” (which ranged from synthetic lavender-scented Febreeze and lotion to low quality essential oils purchased from the local grocery store) with the premium therapeutic essential oils I source for my brands. The following are just some of the findings from these trials. I want to emphasize that while these were simple in-house studies for internal use and were not set up according academic or clinical research standards, they still held immense value.
Anxiety Trial:
A male resident was experiencing agitation, up at night walking, calling out, and even becoming violent at times. He was not responding well to pharmaceutical intervention and staff became concerned the medications were making him worse. They wanted avoid relying on pharmaceuticals if possible.
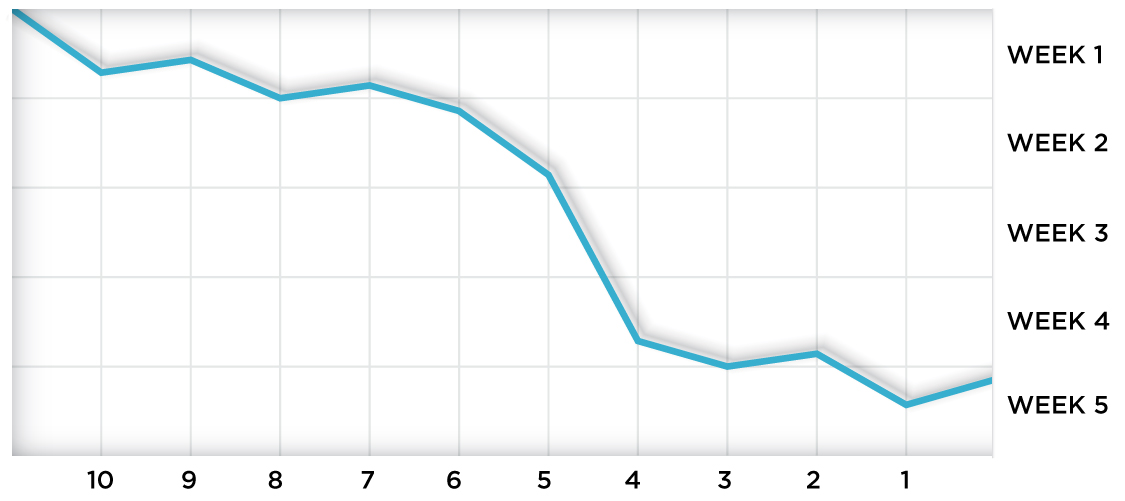
A chart was created to track resident behavior. Behaviors were scaled from 0-10 both before and after aromatic intervention, with a “10” being the worst. Essential oil/blend and method of application were also recorded. We found the following:
The most common method of application was via inhalation. The resident was violent and reactive on several occasions and staff considered him a level 10. During each recorded incident he was successfully calmed after inhalation of our essential oil blend. Results were consistent for this gentleman and staff was able to avoid the use anti-anxiety/antipsychotic pharmaceuticals. Within several weeks he hardly needed the medications. No side effects were reported from the intervention and the staff felt comfortable administering the aromatherapy.
Alcohol Cravings
A gentleman with a history of alcoholism was struggling with his transition into long-term care. He was craving a drink and would exhibit anxious behaviors. In his case, I addressed both the neurological element of addiction and the aroma of the blend. My goal was to mimic the flavor and effect of his favorite drink. This gentleman loved rum and cokes. I blended sweet, spice and vanilla notes with essential oils that were sedative, emotionally balancing and somewhat euphoric. He was provided an inhaler and instructed to use it when he felt a craving. The gentlemen reported that he like the blend and felt it helped him. Staff reported the gentleman would calm down and was better cope with the transition.
WWII Survivor
An elderly woman was admitted into the transitional care unit to recover after a surgery. She was having a difficult time sleeping at night, experiencing symptoms of PTSD including hallucinations and flash backs from World War II. She was also diagnosed with post-operative delirium. The DON was concerned because she was not improving and further medicating was adding to the problem.
In this case I wanted to address her physical pain, her emotional/spiritual state and support deep, quality sleep. The blend included powerful anti-inflammatory essential oils, sedatives and those aromatics historically known for their spiritual significance. I instructed staff to dilute the blend and massage it into her feet and legs, while avoiding her incision site on the knee. The DON called me back after a week of use and said: “Whatever you made, it’s working – and we need more!” This patient’s delirium was calmed, her perception of pain reduced and her sleep improved. She was able to return to a normal sleep/wake cycle and better participate in her recovery from surgery.
Other Positive Results
There is always more than meets the eye during an aromatic intervention. Those working directly with patients often feel helpless when traditional interventions do not work and/or produce more challenges due to negative side-effects. When a simple and non-invasive solution is available to staff, they feel empowered and their stress level is reduced. Having a safe non-pharmaceutical alternative that works without producing side effects allows them to feel more confident and successful in their jobs.
Staff can enjoy the benefits of aromatherapy also. They might use a stimulating blend to perk up during a long shift, take a whiff of their favorite essential oil when unpleasant odors are present, or take advantage of natural anxiety relief when they are having a bad day. They can even relieve debilitating headaches and find relief when feeling under the weather.
In each situation, aromatherapy not only reduced the patient’s symptoms but it also reduced or eliminated the challenges associated with pharmaceuticals (ie: side effects, waiting for them to begin working, wearing off before they can be re-administered). Because the blends are expertly formulated with high quality essential oils, they are safe to use alongside pharmaceuticals. Since aromatherapy is inhaled it directly impacts the brain through the olfactory nerve. Improvement is observed much faster than waiting for a drug that is administered orally to kick in.
We even found the need for a drug was often avoided when aromatherapy was used. The reduced reliance on pharmaceuticals proved to be an invaluable benefit considering now there is stronger regulation in place regarding the use of anti-psychotic and anti-anxiety medications and certain pain relievers. In fact, today the Centers for Medicaid Services require non-pharmaceutical options be utilized in long-term care. Aromatherapy turned out to be the perfect solution.
Perhaps the most important benefit to note is that each resident received tailored care that was gentle, holistic and person-centered without being a major strain on resources or time. Staff simply selected the oil that matched the symptom and administered without the need for a prescription.
The pleasurable impact of aromatherapy quickly reaches the body, mind and soul in a unique and nurturing way. As demand for natural alternatives grow among all consumers today, so does the demand for such care among the aging population as they approach their last stages of life. As we move into the future we will continue to expect long-term care that embraces the needs of the whole person over simply treating their symptoms with medication, as we have seen in the past.
Although these were not official studies, they produced the initial evidence to support my ongoing research and formed the foundation for what I do today. In this case, we used our findings to gain financial support from stakeholders and build a full aromatherapy program for this particular nursing home. We have since expanded my program into their entire health system including assisted living, memory care, and transitional care and they are seeing amazing results. I am proud to see aromatherapy becoming one of the hottest topics in medical literature and know I have been a part of transforming the way we help people age.
In health,